ASTHM 2017 Poster - Achieving global goals for schistosomiasis: rapidly reaching the 2020 and 2025 goals for control and elimination of morbidity
This page is adapted from a poster presented at ASTMH 2017 by Arminder K. Deol, Fiona Fleming, Beatriz Calvo-Urbano, Martin Walker, Victor Bucumi, Issah Gnandou, Edridah Tukahebwa, Samuel Jemu, Upendo J. Mwingira, Abdulhakeem Alkohlani, Mahamadou Traoré, Wendy Harrison, Maria-Gloria Basáñez, Michael D. French, Joanne P. Webster
Introduction
- Schistosomiasis is one of the NTDs with the greatest human health and socio-economic burden
- Approx. 238 million infections, with ~ 90% are in sub-Saharan Africa
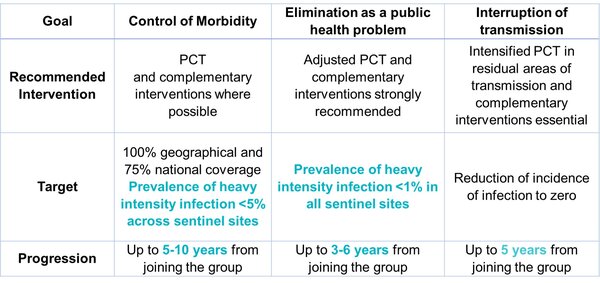
WHO Global Goals for SchistosomiasisControlling Morbidity <5% heavy infections across sentinel sites by 2020 (in all endemic countries) Eliminating as a Public Health (PH) Problem <1% heavy infections in all sentinel sites by 2025 (in all endemic countries) Eliminating Transmission by 2025 (in selected regions) |
This study aimed to address the following questions:
- After how many treatment rounds are 2020 / 2025 targets reached?
- How are routinely-collected Monitoring and Evaluation (M&E) data best used to determine this?
Methods
Multi-country programmatic impact surveys, supported by the Schistosomiasis Control Initiative (SCI), were reanalysed.
We then compared WHO threshold criteria on control and elimination of morbidity (see below table) with the empirical data, to identify whether the current one-size-fits-all approach is optimal for guiding schistosomiasis strategies.
Results
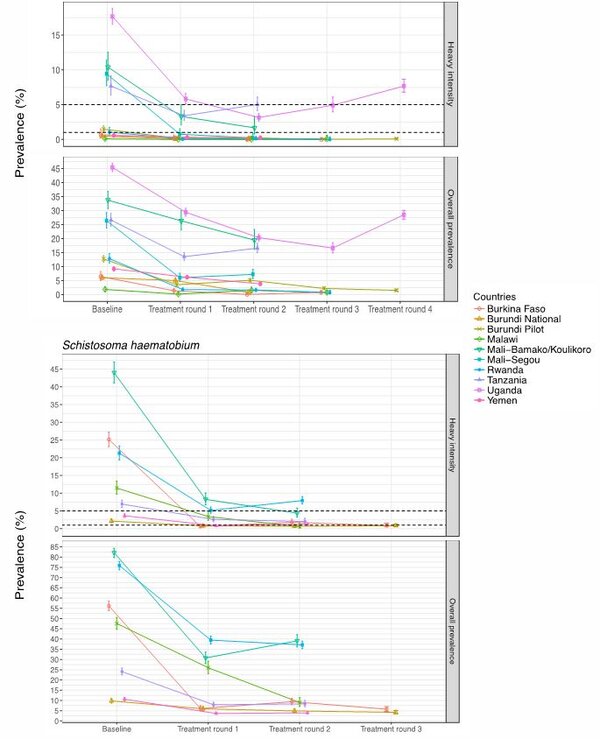
- Country programmes that started with a prevalence of below 5% heavy infection intensity in school-aged children for S. mansoni already reached the goal of control of morbidity and reached elimination as a PH problem in ≤ 3 years.
- For S. haematobium areas, all had high starting endemicities yet all (but one) reached ‘control’ in ≤2years. However none reached the ‘elimination as a PH problem’ target.
- Countries in our study reached ‘control of morbidity’ at earlier time points than anticipated and varied by species.
- Relationship between prevalence of heavy-intensity infection vs overall prevalence was non-linear. A wide range of prevalence values within and between treatment rounds corresponded to <5% heavy-intensity infection.
Conclusions
- As intensity levels decrease with the progression towards elimination, one of the major obstacles we now face is using alternative affordable diagnostic techniques. The current Kato-Katz technique for S. mansoni is not sufficient for this purpose due to its insensitivity at these levels, though the point-of-care urine antigen (CCA) test is a promising tool.
- Many countries have now reached the control aims, esp. for S. mansoni, so the question we now face is what do we do now - continue as before or proceed to the next stage?
- Some countries start with a prevalence of heavy infection <5%.
- The next question is then, what treatment approach should these countries follow – the standard ‘control of morbidity’ or proceed directly too elimination?
Acknowledgements and partners
We’d like to thank the Ministries of Health, the National NTD Programmes, the Monitoring. Evaluation and Research team and other involved team members at the Schistosomiasis Control Initiative (SCI), as well as, the original funders of the surveys and Children’s Investment Fund Foundation (CIFF) for helping to make this study possible.